Cancer Equity For All
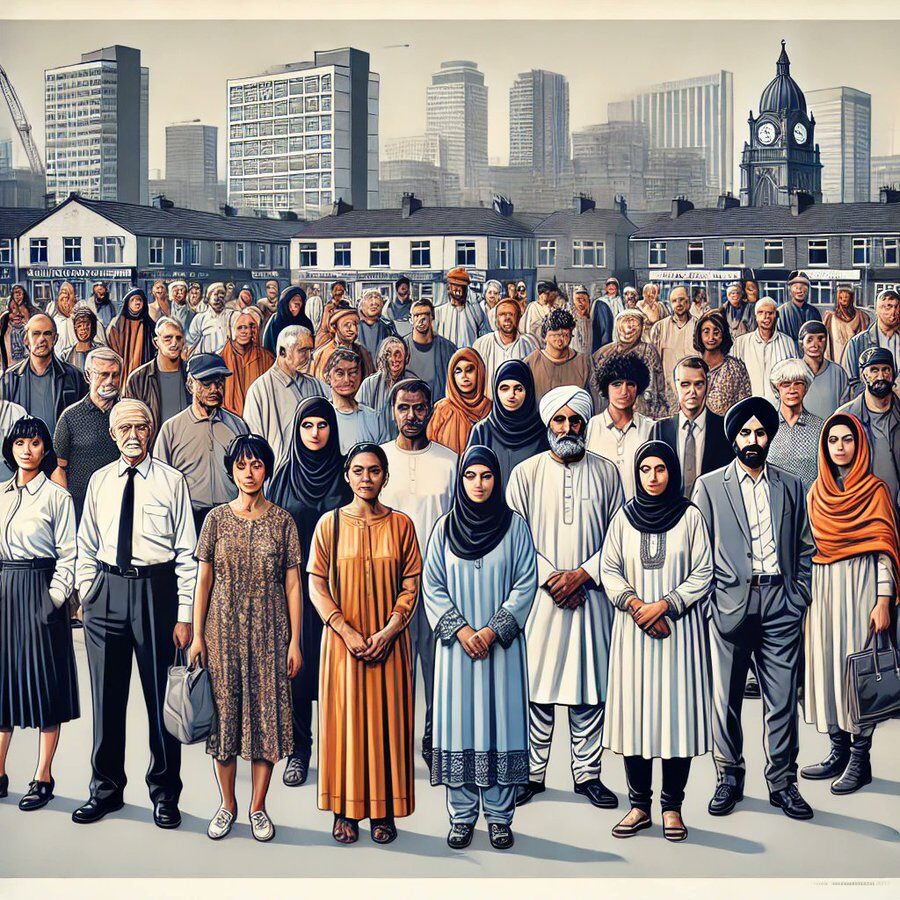
A Shared Challenge
Reality of Health Inequalities
Cancer mortality is 60% higher in England’s most deprived communities compared to affluent areas — driven by a complex mix of social, economic, and healthcare barriers.
Higher rates of emergency admissions
Greater prevalence of long-term conditions, often alongside cancer
Prolonged hospital stays (Length of Stay, LOS)
Higher NHS spending per capita
The Cost of Inequality
How Social Deprivation Drives Poor Health Outcomes
Health inequalities in England are deeply linked to socioeconomic status, ethnicity, and geography. People in the most deprived areas are almost 60% more likely to die from cancer than those in wealthier areas. This inequality is driven by multiple factors, including:
📌 Smoking rates are three times higher in deprived areas, significantly increasing cancer risk.
📌 Obesity is nearly 40% more common in low-income groups due to lack of access to healthy food and exercise facilities.
📌 Limited health literacy delays diagnosis and reduces access to life-saving treatments.
📌 Financial strain forces people to skip medical appointments due to transport costs or problems with taking time off work.
The cost-of-living crisis has worsened these challenges, particularly for socially deprived communities, white working-class populations, ethnic minorities, disabled individuals, neurodiverse people, LGBTQ+ groups, and others facing barriers to care.
Without targeted interventions, these inequalities will continue to widen.
Every 4 minutes, someone in the UK dies from cancer
New UK Cancer Cases (Annual)
375,000 per year | 7,211 per week | 1,027 per day
Cancer Deaths Annually: 167,142
Survival (10+ years): 50%
Preventable Cases: 38%
Annual NHS Cancer Service Costs: £5 billion
The Business Case for Reducing Health Inequalities
The Financial Impact
£5 billion Increased NHS Treatment Costs
£31 billion Productivity Losses
£20 billion Lost Tax Revenue & Higher Welfare Payments

Advancing Cancer Equity for All
Achieving cancer equity begins with knowledge, awareness, and action. We are committed to empowering healthcare and oncology professionals with the tools they need to recognise, address, and reduce disparities in cancer care — and to communicate in an equitable, accessible, and culturally competent way.
Our work focuses exclusively on cancer equity, ensuring that professionals:
✔ Understand the barriers to equitable cancer care and how to overcome them.
✔ Engage meaningfully with underserved and marginalised communities.
✔ Have the right conversations — internally within the NHS and cancer care networks, and externally with patients, the public, and advocacy groups.
✔ Communicate complex cancer information in ways that are clear, inclusive, and accessible — tailored to different literacy levels, cultural contexts, and needs.
By transforming how cancer information is delivered, understood, and acted upon, we are shaping a healthcare system that works for everyone, not just the few.
IMPROVEMENTS MADE
INEQUALITY REMAINS
Despite advances in cancer care, access remains unequal — worsening disparities in survival and patient outcomes.
For patients from underrepresented communities, barriers exist not only in access but in how care is discussed and decisions are made.
To achieve cancer equity for all, the NHS must go beyond representation and actively engage communities where they are, ensuring no one is left behind in the future of personalised cancer care.
